December 23, 2023
The Honorable Kathy Hochul
Governor of New York State
NYS State Capitol Building
Albany, NY 12224
Dear Governor Hochul,
I watched with interest the news that “Grieving families across New York are fighting
what they call an injustice”. The
decades old law that limits payouts in wrongful death lawsuits based on the
persons age and / or financial worth. https://www.cbsnews.com/newyork/news/new-york-grieving-families-act/
This fight has been going on
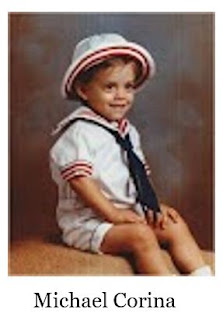
so long and I for one, lived it when my young son bled to death following a
tonsillectomy over 30 years ago. I didn’t
need the money, my son was dead, I wanted answers as to how this happened and
without a lawsuit, no one would talk. There
is an important piece missing. The
lawsuit happens after the death. We need
to avoid the death to begin with and one reason I believe death from medical
errors are so high is because the public is not prepared to be patients.
In 1996 we started Pulse Center
for Patient Safety Education & Advocacy a small grassroots organization
based on Long Island, New York to educate the public to be a support and
advocate for each other for the best outcomes in care. Learning how errors happen (something many
survivors want to know) and how to avoid medical injury needs the attention we
have never received. Whether it is for older
adults, cancer, lupus, epilepsy, mental illness, disabilities, broken bones or
rare diseases, learning patient advocacy can save lives and reduce lawsuits
following death or injury. So, while there is a discussion about payment after
a wrongful death, please consider the work we have been doing for 25 years to
avoid the injuries and death within the healthcare system, by educating the
public to begin with.
Sincerely. Ilene Corina,
BCPA
President, Pulse Center
for Patient Safety Education & Advocacy
www.PulseCenterforPatientSafety.org
516.579.4711