When Things Go Wrong, Is it About Blame?
Thirty-five
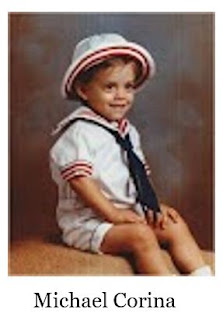
years ago, like many other children and even adults, my only child at the time
had chronic ear infections. It was
suggested by three different doctors (I got three opinions) that he needed his
tonsils removed. I chose the “nicest” doctor
who himself had a daughter my son Michaels age. After the surgery, for a full
week, he was bleeding. Sometimes a lot,
sometimes a little but each time I saw blood, I went to a hospital or urgent
care. Even at the one week follow up, the surgeon said he was fine. The
following day, Michael died from blood loss and a body full of infection. All signs were missed by 5 doctors and his
surgeon. Oh well, it’s too late to turn back the clock.
No one ever
asked what I saw went wrong. What could
I have done differently? All the “blame”
was on the doctors and yes even the nurses who saw him. If I knew then what I know now, could Michael
be alive? I will never know. We can’t
measure the positive outcomes. When things
go right, well everyone is expecting that but when it goes wrong, all doors get
closed.
So, as we
come to another Patient Safety Awareness Week, remember that we, all of us who
use the healthcare system have some responsibility to practice safe care
through education and awareness. Please
learn what you can and don’t be a passive partner in patient safety. Be aware and involved and let’s fix the system
through our behavior and let those who work in healthcare fix it from within.